
WILLIAM RAU
I know three people who collapsed from heat stroke. Doctors told frantic parents of two kids to immerse them in a cold-water bath. The third, a high school runner who collapsed during a race, attended a school where the athletics department had an ice tub. He too was immersed in cold water. All three are healthy and productive. Rapid immersion in cold water prevented damage to their brains and other organs.
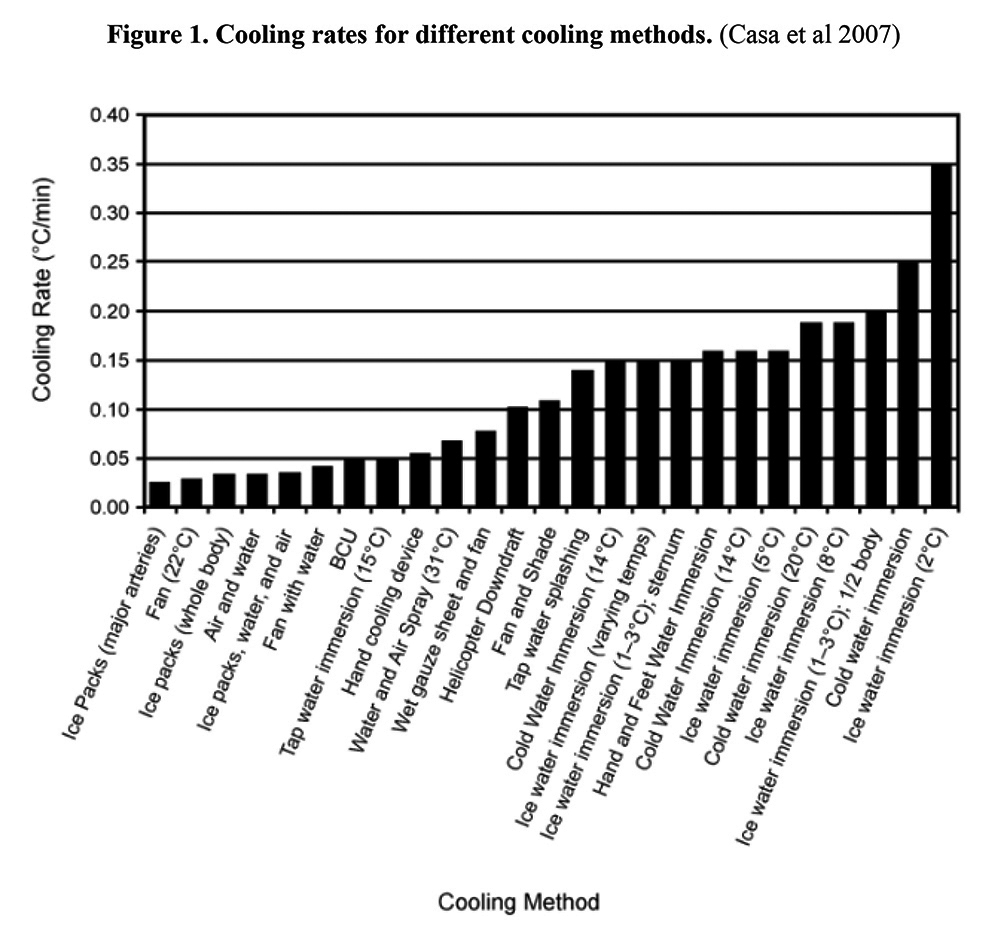
As Figure 1 shows, cold water or ice water immersion is the fastest method for cooling a dangerously overheated body. And minutes can make the difference between full recovery versus multiple organ damage or death. That is why immediate, full-body immersion in cold water is now the gold standard treatment for exertional heat stroke. To avoid overcooling, gold standard practitioners monitor cool-down with a special rectal thermometer and remove victims from cold water once normal body temperatures are achieved.
Unfortunately, County Emergency Medical Staff in Central Illinois wrote heat stroke protocols that default to “transport first, treat second” approaches. Heat stroke victims are transported to emergency rooms as quickly as possible with treatment turned over to ER doctors. This is OK with rapid transport of early-stage victims as long as physicians and cooling tubs are immediately available. It is NOT OK during a big heat wave, or pandemic, since the number of heat stroke patients that must be treated immediately will overwhelm ERs. Things will be much worse if a heat wave crashes the grid or big power plants resulting in widespread loss of air conditioning.
Protocols move victims to a cool place (good, especially rooms at 62°F to 68°F), but then specify placing cold-packs on central pulse points or arteries. A cold pack, Figure 1 shows, is the least effective cooling method. These cold packs are placebo treatments –– medical fakery in essence –– and are probably used to calm distressed relatives rather than treat patients. Complicating matters further, the protocols do not require an objective measure of heat stroke with a rectal thermometer, the only fully accurate means of doing so. Paramedics are left to guess rather than rely on an instrument they are trained to use. These deficient protocols can cause paramedics to miss heat stroke because not everyone with a temperature above 104°F displays the signs of such organ-destroying heat.
Paramedic vans can’t carry around tubs; they don’t have to. The lion’s share of heat stroke happens in or near buildings that have tubs, showers, or cold, running water. Field treatment of exertional heat stroke is literally a sustained dunk in cold water. Treatment for the elderly (classic heat stroke) is less certain because heat stroke research is tied to sports and military medicine. Is cooling by an evaporation technique or cold-water immersion best for the elderly? Experts don’t know, but none call for cold packs.
County emergency medical staff, the protocol writers, need to become familiar with science-based heat stroke research. Like cardiac arrest, we need to move initial treatment of heat stroke into the field.
William Rau is Illinois State University professor emeritus of sociology.

Recent Comments